Introduction to Bioceramic Pulp Caps
A bioceramic pulp cap is a protective layer placed over the dental pulp when it is nearly exposed or has a small, clean exposure. The goal is to keep the pulp alive, reduce bacteria, and help the tooth repair itself. In a common scenario, a deep cavity is cleaned and a tiny spot of pulp shows. A bioceramic material is placed, then the tooth is restored.
Bioceramic materials are calcium silicate based and are highly biocompatible. They release calcium ions, have a high pH, and encourage mineral formation at the pulp surface. This environment supports healing and can lead to a dentin bridge, a natural barrier that protects the pulp. These materials also seal well, which limits microleakage. Good sealing helps keep bacteria out while the pulp recovers.
Success starts with correct diagnosis and case selection. The tooth should have symptoms of reversible pulpitis or no pain, respond normally to cold tests, and show no signs of lingering pain or swelling. Hemostasis after a gentle pulp exposure, usually with a disinfecting solution, is important before placing the bioceramic. Clean technique, rubber dam isolation, and a well-sealed final restoration are essential steps. If the pulp is irreversibly inflamed or necrotic, a different approach like modern root canal treatment is usually more appropriate.
For patients, a bioceramic pulp cap can preserve the natural tooth and avoid more invasive treatment. Expect the tooth to feel normal or slightly sensitive for a short time, then settle as healing occurs. Follow-up visits allow your dentist to confirm normal responses and healthy tissue over time. Dentists use bioceramic pulp caps because they combine a strong seal with a biologic boost for healing. Clinicians also follow bioceramic pulp cap guidelines to standardize selection, placement, and follow-up. Preserving pulp health often leads to better long-term tooth function.
Indications for Vital Pulp Therapy
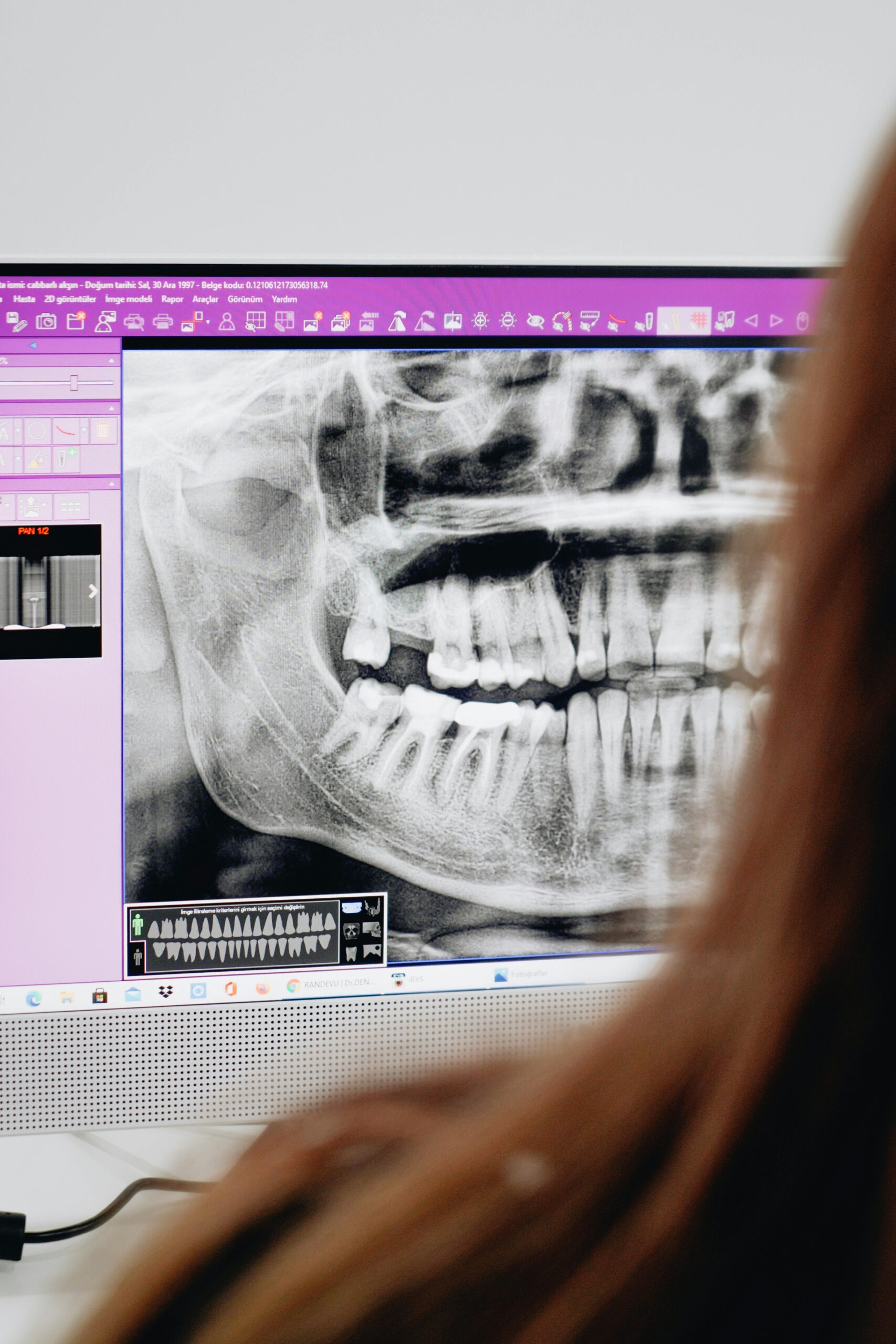
Vital pulp therapy is indicated when the pulp is alive and capable of healing. Typical candidates include teeth with deep decay or a small mechanical exposure where bleeding can be controlled, with no swelling or sinus tract. The tooth should have no spontaneous pain or only brief cold sensitivity, suggesting reversible inflammation. Radiographs should show no apical pathology and roots adequate for function.
A cusp breaks on an olive pit, exposing a pinpoint pulp spot. In practice, the tooth should respond to cold without lingering pain, and be non-tender to biting and percussion. Controlled hemostasis in a short time, often within a few minutes, supports a favorable inflammatory state. Bright red, modest bleeding that stops with gentle irrigation is preferred; persistent or dark bleeding may signal deeper disease. Because the material choice matters, calcium silicate cements that stimulate pulp cells and reparative dentin formation support these indications and improve biologic predictability [1].
Most bioceramic pulp cap guidelines converge on the following practical indications:
- Deep caries with normal or reversible symptoms after careful caries removal.
- Small, clean mechanical exposure during preparation or minor trauma without gross contamination.
- Carious exposure where a partial or full coronal pulpotomy achieves hemostasis within a few minutes.
- Immature permanent teeth needing continued root development and apexogenesis.
- Teeth without periapical radiolucency, swelling, or sinus tract on exam.
- Cases that allow rubber dam isolation and immediate, high‑quality coronal seal.
For patients, these indications mean your dentist is selecting cases where healing is likely and more invasive therapy can often be avoided. After treatment, the tooth should be sealed the same visit, sometimes followed by a protective restoration such as a protective dental crown if structure is heavily compromised. Follow-up checks confirm normal responses and continued comfort. The right case selection protects pulp health and tooth longevity.
Selection Criteria for Bioceramic Pulp Caps
Choose a bioceramic pulp cap when the pulp is healthy enough to heal and the tooth can be sealed well. The tooth should test normal or show reversible sensitivity, with no swelling, sinus tract, or tenderness to biting. Radiographs should show no apical radiolucency. Most bioceramic pulp cap guidelines emphasize quick bleeding control, clean conditions, and a durable final restoration.
A small, clean exposure is preferred, whether carious, mechanical, or traumatic. A real-world example: a tiny pinpoint exposure appears after careful caries removal. Bleeding should be bright red and stop in a short time with gentle irrigation. Fast hemostasis suggests mild inflammation and a better chance for dentin bridge formation. If bleeding is profuse, dark, or persists despite proper steps, the pulp may be more inflamed than a simple cap can manage.
Diagnosis leads the decision. Teeth with spontaneous pain, lingering cold pain, or percussion tenderness are poor candidates. So are teeth with deep cracks into the pulp, large uncontrolled caries, or suspected necrosis. In contrast, a normal cold response, no night pain, and no apical changes support conservative care. Age is not a strict limit, but younger pulps often heal faster, especially in immature teeth.
Isolation and sealing are equally important. A rubber dam, disinfected field, and immediate placement of a bonded restoration limit bacterial leakage. The tooth must be restorable, with margins on sound tooth and occlusion that will not overload the repair. If much tooth structure is missing, plan protective coverage to reduce fracture risk and protect the pulp cap.
Treatment choice also depends on exposure size and caries depth. A pinpoint exposure with quick hemostasis may suit a direct cap. A wider or inflamed exposure may benefit from a partial pulpotomy to reach healthy pulp before placing the bioceramic. These criteria help clinicians match the procedure to the tissue state and improve outcomes. Thoughtful selection protects pulp vitality.
Advantages of Using Bioceramics
Bioceramic materials support pulp healing while creating a durable seal against bacteria. They are kind to living tissue, help new mineral form, and work well in the moist conditions often present after careful caries removal. Many can be placed and covered with a final restoration in one visit. These advantages make them a strong choice when the goal is to keep the pulp alive.
Bioceramics release calcium ions that stimulate pulp cells to lay down protective hard tissue. Their naturally high pH creates an environment that is less friendly to bacteria, which lowers the risk of infection during healing. At the interface, they can form hydroxyapatite and micromechanical tags, improving adaptation and limiting microleakage. Low solubility and dimensional stability help the material maintain its seal over time. Radiopacity allows clear follow-up on radiographs without guessing.
In practice, these properties simplify the appointment and support success. Moisture tolerance means controlled bleeding and gentle irrigation do not undermine the material’s seal. Shorter setting times in modern formulations allow predictable layering of a bonded restoration soon after placement. Many bioceramics also show better color stability than older options, reducing the chance of darkening in esthetic areas. A brief real-world example: after a small pulp exposure, a dentist caps it and restores the tooth the same visit.
Clinically, bioceramics fit conservative strategies. They allow direct caps for tiny, clean exposures, and they pair well with partial pulpotomy when a slightly deeper removal is needed to reach healthy tissue. In immature teeth, their biologic activity supports continued root development, which improves long-term tooth strength. For patients, the benefits translate to preserved vitality, fewer invasive steps, and a normal-feeling tooth after healing. Many bioceramic pulp cap guidelines highlight these benefits as they standardize selection, placement, and follow-up. The key takeaway: bioceramics protect the pulp while helping it repair itself.
Application Techniques for Pulp Caps
Pulp caps are placed in a clean, dry field to protect a small pulp exposure and help it heal. The basic steps are isolation, gentle cleaning, controlled bleeding, placement of a bioceramic layer, and a well-sealed final restoration. When done carefully, these steps keep bacteria out and give the pulp a chance to repair. A small carious exposure appears while removing deep decay.
Start with anesthesia and rubber dam isolation so saliva and moisture do not reach the site. Remove softened dentin and stop when the exposure is clean and pinpoint. Achieve hemostasis with a gentle irrigant, often a small amount of sodium hypochlorite on a cotton pellet for a short time. Bleeding should turn bright red and stop within a few minutes; if it does not, consider removing 1 to 3 millimeters of inflamed tissue as a partial pulpotomy before trying again. Rinse lightly, avoid strong air blasts on the pulp, and confirm a quiet, controlled surface before placing material.
Place the bioceramic in a thin, uniform layer, usually about 1 to 2 millimeters over the exposure and onto surrounding sound dentin. Do not pack hard; gentle adaptation avoids forcing material into the pulp. Allow initial set as directed, then cover with a protective base if needed and proceed to a bonded restoration the same visit. Keep etchants and primers off unset bioceramic; use careful technique so the seal is not disturbed. Avoid eugenol materials, which can interfere with resin bonding near the cap.
For a partial pulpotomy, create a shallow, flat cut into coronal pulp until bleeding is controlled and bright. Rinse, obtain hemostasis, then cap the wider surface with bioceramic, extending onto dentin for a reliable seal. Restore immediately with a durable coronal seal and adjust the bite to reduce heavy contacts. Most bioceramic pulp cap guidelines emphasize isolation, sodium hypochlorite hemostasis, adequate material thickness, and immediate definitive restoration to limit leakage.
For patients, these steps shorten visits and protect comfort while preserving the tooth. If dental anxiety is a concern, gentle oral sedation options for restorative care can help. The key takeaway: precise steps and a strong seal give the pulp the best chance to heal.
Post-Treatment Considerations
After a bioceramic pulp cap, most patients feel mild, short‑lived sensitivity to cold or chewing. This usually improves over several days as the pulp settles and the restoration seals the tooth. Avoid hard biting on the treated tooth until it feels normal. Contact your dentist if pain wakes you at night or swelling appears.
After a cap, a patient notices brief cold sensitivity that fades over days. Early healing involves calming the pulp and keeping bacteria out with a tight coronal seal. If a temporary material was placed, a timely definitive restoration protects the repair and reduces fracture risk. Your dentist may also fine‑tune the bite so one tooth is not carrying extra force, which can prolong sensitivity.
Follow‑up checks confirm that the pulp remains healthy. Many bioceramic pulp cap guidelines suggest a short recall, often around 6 to 8 weeks, then periodic reviews over 6 to 12 months. At these visits, your dentist looks for normal responses to cold, lack of tenderness to biting, and stable radiographs. Over time, a hard tissue barrier may form beneath the cap, and the tooth should feel normal in daily function. In contrast, lingering cold pain, spontaneous pain, swelling, a sinus tract, or a new radiolucency can signal failure and the need to reassess treatment.
Home care supports healing. Brush and floss gently around the tooth to limit plaque, and avoid chewing very hard foods on it until fully restored. If a large portion of tooth is missing, protective coverage may be planned to prevent cracks. If symptoms worsen or persist beyond a few days, schedule an evaluation during our current hours. Thoughtful follow‑up and a durable seal give the pulp the best chance to stay healthy.
Follow-Up Guidelines for Success
Plan a short follow-up after a bioceramic pulp cap to confirm healing, then space visits as the tooth stabilizes. A common schedule is a clinical check at 6 to 8 weeks, another review around 6 to 12 months, then yearly if stable. At each visit, assess symptoms, perform sensibility testing, check the bite, and evaluate the restoration seal. Take a baseline radiograph soon after treatment and compare at later visits if changes are suspected.
Early visits focus on comfort and pulp responses. Brief cold sensitivity that fades quickly is typical; lingering cold pain suggests ongoing inflammation and needs attention. No response to cold can occur under thick restorations, so retest with control teeth and consider alternative tests. As healing progresses, expect a normal or reducing cold response, no tenderness to biting, and a quiet soft tissue exam. A short real-world example: mild cold zings for a week, then the tooth feels normal.
Radiographic review looks for stability. Lack of new periapical radiolucency supports success, and a dentin bridge may appear over time, although its absence alone does not mean failure. The restoration seal is critical at every visit; even small margin defects can allow leakage. If a localized edge is open, consider prompt repair with conservative dental bonding repairs to protect the cap. Occlusion should be balanced so the treated tooth does not carry heavy contacts that can prolong sensitivity.
Document key details to guide decisions. Record the initial diagnosis, exposure size, time to hemostasis, material placed, and the type of final restoration. Note each follow-up response to cold, percussion, and biting, and compare to baseline. If signs point away from healing, such as spontaneous pain, night pain, swelling, a sinus tract, or a new radiolucency, escalate promptly. Options include a partial pulpotomy to reach healthier tissue or referral for endodontic care, depending on symptoms and tests.
These steps align with bioceramic pulp cap guidelines and help the pulp stay healthy long term. For patients, clear follow-up and a well-sealed restoration give the tooth its best chance to remain comfortable and functional.
Potential Complications and Management
Complications after a bioceramic pulp cap can include prolonged sensitivity, lingering inflammation or pulp death, leakage around the restoration, staining, and tooth fracture. Management depends on the cause. Many problems resolve with bite adjustment, sealing small margin gaps, or brief symptom care. If signs point to irreversible pulpitis or necrosis, endodontic treatment is usually indicated.
A real-world example: after a deep filling, the tooth aches with cold for 30 seconds. Short, improving sensitivity over days is common. Pain that lingers more than a minute, wakes you at night, or appears without a trigger suggests the pulp is not recovering. In that case, the plan should be reassessed rather than waiting.
If the tooth feels high, an occlusal adjustment often relieves biting tenderness. Mild discomfort can be managed with a short course of over‑the‑counter pain control as advised by your dentist. If the restoration edge is slightly open, repairing the margin or replacing the restoration can stop leakage and calm the pulp. Clear communication about what is normal, and what is not, helps patients know when to call.
Intraoperative challenges matter. If bleeding could not be controlled quickly at the first visit, a partial pulpotomy to reach healthier tissue often improves outcomes before placing bioceramic. If the field was contaminated, re‑isolate, gently disinfect, and re‑establish a clean surface. When hemostasis is not achievable or pain persists despite correct steps, change course and consider definitive endodontic care.
Other potential issues include internal calcification that can reduce future canal size, usually monitored unless symptoms develop. Some materials may discolor thin anterior enamel; careful material selection and sealing techniques reduce this risk. Teeth with large structural loss are prone to fracture, so timely cuspal coverage can protect the repair. These decisions align with bioceramic pulp cap guidelines that emphasize diagnosis, a tight seal, and timely intervention when healing does not progress.
For patients, most problems are manageable when noticed early, and a quick check can prevent bigger steps later. Early recognition and simple fixes often restore comfort.
Frequently Asked Questions
Here are quick answers to common questions people have about Vital Pulp Therapy With Bioceramics in Glendale, AZ.
- What is a bioceramic pulp cap?
A bioceramic pulp cap is a protective layer used in dentistry to cover the dental pulp when it is almost exposed. Its purpose is to keep the pulp alive, reduce bacteria, and aid in the tooth’s self-repair. Made from calcium silicate, these materials are biocompatible and release calcium ions, fostering healing and leading to the formation of a dentin bridge, which serves as a natural barrier to protect the pulp.
- When is vital pulp therapy indicated?
Vital pulp therapy is indicated in cases where the pulp is alive and can heal. Candidates include teeth with deep decay or minor mechanical exposure. There should be no swelling or sinus tract, and the tooth should exhibit reversible pulpitis symptoms like brief cold sensitivity. Controlled bleeding without lingering pain after careful caries removal is essential for this therapy to be considered successful.
- How do bioceramic materials help prevent bacterial leakage?
Bioceramic materials create a durable seal against bacteria, which is crucial for pulp protection. Their naturally high pH environment helps prevent infection during healing. At the material-dentin interface, bioceramics form hydroxyapatite and micromechanical tags that enhance adaptation and limit microleakage, maintaining their seal over time [ref:40423766].
- What are the advantages of using bioceramics in pulp therapy?
Bioceramics offer several advantages in pulp therapy. They support pulp healing and create a strong barrier against bacteria, encouraging new mineral formation. Bioceramic materials work well in moist environments, release calcium ions, and boast low solubility, ensuring their stability over time. Many formulations allow for one-visit placement and restoration, simplifying the process for both dentists and patients.
- What are the initial steps in placing a bioceramic pulp cap?
To place a bioceramic pulp cap, begin with anesthesia and rubber dam isolation to maintain a clean field. Remove softened dentin until the area is clean. Control the bleeding with gentle irrigation, often using sodium hypochlorite. Once bleeding is controlled, place the bioceramic material over the exposure and surrounding dentin, followed by a well-sealed final restoration to ensure the pulp is well-protected.
- How effective are bioceramic pulp caps in promoting healing?
Bioceramic pulp caps are effective in promoting healing by creating an environment conducive to tissue repair and protection. Their calcium ion release stimulates pulp cells to form a hard tissue barrier, enhancing the self-repair process. This makes them a reliable choice for cases where pulp vitality can be preserved, contributing to better long-term tooth function [ref:38701294].
- What follow-up care is required after a bioceramic pulp cap is placed?
After placing a bioceramic pulp cap, follow-up visits are needed to ensure healing. Initial visits might be scheduled at 6 to 8 weeks, followed by periodic reviews every 6 to 12 months. During these visits, your dentist will check symptoms, perform sensibility testing, and assess the restoration’s seal. Monitoring ensures that the pulp remains healthy, and timely intervention can be made if issues arise.
References
- [1] In Vitro Response of Dental Pulp Stem Cells to Calcium Silicate-Based Cements: A Systematic Review and Meta-Analysis of Preclinical Evidence. (2025) — PubMed:40895876 / DOI: 10.7759/cureus.88990